Abstract
Antihypertensive medication treatment is one effective management strategy to prevent cardiovascular disease (CVD) and mortality. However, little research has been conducted on the rates of antihypertensive medication adherence and the effect of antihypertensive medication adherence on health outcomes in South Korea. We searched the Korean National Health Insurance Claims Database for records from 2003 to 2007. Patients in this study were 18 years of age or older and they were diagnosed with hypertension and newly prescribed antihypertensive medication in 2003. Adherence to antihypertensive medication was estimated as the medication possession ratio (MPR). Multivariate Cox regression was used to evaluate the association between medication adherence and adverse health outcomes after adjusting for patient demographics and clinical characteristics. Our study population consisted of 40 408 patients with a mean age of 51 years. Among the patients, 50.3% were men, 4.0% had Medicaid health insurance, 17.8% had diabetes, 20.9% had dyslipidemia and 42.4% were adherent (MPR ⩾80%). Nonadherent patients (MPR<80%) were younger and more likely to have Medicaid health insurance; they had lower rates of diabetes and dyslipidemia compared with adherent patients. In the Cox multivariate analysis, nonadherence increased the risk of all adverse health outcomes, including all-cause mortality and hospitalization for CVD (hazard ratio: 1.57, confidence interval: 1.40–1.76). In conclusion, our study indicates that medication adherence is important for reducing hospitalization due to CVD and mortality.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are the major leading cause of death in the world. Hypertension is one of the main risk factors for CVD, and managing blood pressure in hypertensive patients is important for the prevention of CVD and mortality. One effective management strategy to control blood pressure is medication. Patients who are adherent to antihypertensive drugs are more likely to achieve blood pressure control, have a decreased risk of adverse outcomes, including all-cause hospitalization, CVD hospitalization, revascularization of CVD, all-cause mortality and CVD mortality, and have lower health-care costs compared with patients with low adherence.1, 2, 3, 4, 5, 6, 7, 8
However, little research has been conducted on the rates of long-term antihypertensive medication adherence and the effect of antihypertensive medication adherence on adverse health outcomes in hypertensive patients in South Korea.9, 10 In addition, previous studies on the association between medication adherence and health outcomes have used limited study populations or a small number of patients in clinical settings.2, 3, 5, 6 Considering the differences in disease distribution, disease risk and healthcare systems between countries, it may not be appropriate to apply the results of previous studies to the interpretation of problems related to CVD and the design of interventions for improving health outcomes in hypertensive patients in South Korea.
The objectives of this study were to assess the long-term medication adherence rates of hypertensive patients who were newly prescribed antihypertensive medication in South Korea and to evaluate the effect of adherence to antihypertensive medication on all-cause mortality and hospitalization for CVD.
Methods
Data collection
Our study used secondary data such as the Korean National Health Insurance Claims Database (KNHICD), which was established to review claims data and assess quality of care in South Korea. Our country has a national health insurance system and a single insurer to cover all South Koreans; therefore, the KNHICD database is not limited to specific geographical areas, hospitals or patients, and it contains all information for all South Korean patients who use medical services.
The KNHICD contains information for inpatient or ambulatory services (for example, visit dates, diagnosis codes classified according to the International Classification of Disease, 10th Revision (ICD-10) given by physicians, surgery or treatment codes provided to patients, length of stay in hospitals, health-care costs), prescriptions (for example, date, drug name, dosage, cost) and patient characteristics (for example, age, gender, type of insurance). In addition, we merged this database with the health insurance qualification database to include mortality information. However, this database does not contain patients’ cause of death; using this database, we could only identify whether patients had died.
All patient identifier number codes were changed into anonymous numeric codes and names were deleted to protect private patient information. Our research was approved by the Health Insurance Review and Assessment Service Ethics Committee.
Study population
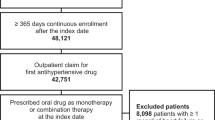
We focused on the patients who had a hypertension diagnosis and took antihypertensive medication to evaluate associations between antihypertensive medication adherence and outcomes. In 2003, there were 969 884 diagnosed hypertensive patients who had at least two claims for outpatient services or one claim for hospitalization with a hypertension diagnosis (ICD-10: I10, I11, I12, I13 or I15) in 2003 and had no medical utilization with hypertension during the 12 months preceding the first diagnosis date. We randomly sampled 10% (96 988) of the 969 884 diagnosed hypertensive patients. Patients who were 18 years of age or older and had at least one prescription for any antihypertensive drug (calcium channel blockers, diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, beta-blockers or a combination) in 2003 were included as the study population. We defined this study population as patients who were newly prescribed antihypertensive medications. We observed the study population from 31 January 2003 to 31 December 2007.
Further, patients were excluded from the study population if they died or were hospitalized with any CVD (ischemic heart disease (IHD; ICD-10: I20–I25), stroke (ICD-10: I60–I64) or chronic heart failure (ICD-10: I42, I50) within 1 year of the index date, which was defined as the date of the first prescription for hypertension medication because we needed sufficient observation time to evaluate the effect of adherence to antihypertensive medication on health outcomes.
Assessment of medication adherence
We used secondary data to evaluate adherence to antihypertensive medication in a real-world setting. Adherence to antihypertensive medication was measured as the medication possession ratio (MPR) based on the ratio of the number of days supplied with medication in the study period to the total number of days in the study period.11, 12 The differences in MPR values between patients are based on the number of days of the prescription for antihypertensive medications in the study period.12 For example, if a patient was supplied with medication for 100 days of 1 year, then the MPR was calculated as 27.4% ((100 days/365 days) × 100). An MPR of 1 (full adherence) indicates that the number of days supplied is equal to the number of days in the period. The MPR method is the best available measurement of medication adherence using administrative data.4, 11, 13
In our study, the MPR was calculated as the ratio of the total number of days for which antihypertensive medication was supplied to a patient during the patient’s study period to the total number of days in the patient’s study period.4, 11, 13, 14 The study period of each patient in our study was determined as the time from the index date to all-cause mortality, first hospitalization for CVD or 31 December 2007, whichever occurred first.
On the basis of the previous studies, adherence to antihypertensive medication was defined as an MPR⩾80% and nonadherence to antihypertensive medication was defined as an MPR<80%.4, 11, 15, 16 Patients who took <80% of their antihypertensive medications had a higher risk of CVD hospitalization and poor blood pressure control compared with adherent patients (⩾80%). We used the 80% cutoff point to classify patients as adherent or nonadherent, as supported by empirical evidence.11, 16 We used a categorized adherence instead of continuous adherence because this cutoff point helps to easily identify patients who require intervention to improve medication adherence.
Health outcomes
The main outcomes were hospitalization for CVD (IHD, stroke and chronic heart failure) and all-cause mortality. Hospitalization for CVD was determined when patients received medical services as inpatients or in the emergency room with a primary diagnosis code for CVD. All outcomes were recorded as dichotomous variables.
Covariates
We collected relevant information that could affect CVD hospitalization or mortality: age, gender, type of health insurance, cardiovascular risk at baseline, diabetes, dyslipidemia, Charlson’s comorbidity score, the number of classes of antihypertensive medications given upon initial prescription and previous hospitalizations.
Age, gender, type of insurance and the number of classes of antihypertensive medications were assessed at the index date. Patients diagnosed with CVD within 1 year before the index date were considered the high CVD risk group at baseline. Patients with diabetes or dyslipidemia were defined as patients who were diagnosed with diabetes or dyslipidemia and were prescribed antihyperglycemic or antihyperlipidemic medication at the same time. Patient data regarding diabetes, dyslipidemia and Charlson’s comorbidity score were identified during the period starting from 1 year before the index date to the end of the study period. We evaluated data within 1 year before the index date to identify whether patients had a history of hospitalization.
Statistical methods
We used the t-test, χ2-test and analysis of variance to compare differences in baseline characteristics between adherent and nonadherent patients. Predictors of nonadherence to antihypertensive medication were estimated through a multivariate logistic regression model and reported as odds ratios (ORs) and 95% confidence intervals (CIs). After testing the proportionality assumption, Cox’s proportional hazards regression analysis was used to analyze the association between medication adherence to antihypertensive medication and adverse health outcomes, including all-cause mortality and hospitalization for CVD. We also separately estimated the hazard ratios (HRs) of all-cause mortality, hospitalization for CVD, hospitalization for stroke and hospitalization for IHD by applying the same methods.17
The HR estimate represents the risk of hospitalization for CVD or all-cause mortality associated with medication adherence. Patients who did not have an outcome were censored. All multivariate models were adjusted for the covariates listed above.
Analyses were performed using the statistical package software SAS version 9.1 for windows (SAS Institute INC., Seoul, South Korea). All tests were two sided, and statistical significance was defined as a P-value<0.05.
Results
Characteristics of the study population
A total of 40 408 patients were selected as the target population in this study (Figure 1). With regard to study population characteristics, patients were evenly balanced between men (50.3%) and women (49.7%). Approximately half of the patients were middle aged (45–64 years of age) on the index date, and the mean age of the study population was 51 years. As for comorbidities, only 1.7% of the study population were diagnosed with CVD within 1 year before the index date, 17.8% of the study population had diabetes and 20.9% of the study population had dyslipidemia during the period of 1 year before the index date to the end of the study. Among the study population, 7.6% had a history of hospitalization within 1 year before the index date and 75.3% took only one class of antihypertensive medication as their first antihypertensive prescription (Table 1).
Predictors of nonadherence to antihypertensive medication
Adherence, defined as a medication adherence⩾80%, was achieved by 42.4% of the study population (Table 1), and the mean overall adherence during the follow-up periods of the study population was 57.9% (median: 70.8%, data not shown). Adherent patients were older, were more likely to have diabetes or dyslipidemia, had fewer prior hospitalizations and took more than two different classes of antihypertensive medications at the index date.
Table 2 shows the predictors affecting nonadherence to antihypertensive medications using a multivariate logistic regression model (C-statistics: 0.61). The risk of nonadherence was relatively low in patients who were old (45–64 years: OR=0.54, CI=0.52–0.57; 65+ years: OR=0.60, CI=0.57–0.64), had Medicare health insurance (OR=0.86, CI=0.78–0.96), had diabetes (OR=0.66, CI=0.62–0.69) and/or had dyslipidemia (OR=0.67, CI=0.62–0.68). Patients with a history of hospitalization showed a higher risk of nonadherence (OR=1.35, CI=1.25–1.47) than patients without a history of hospitalization. Patients taking more than two different classes of antihypertensive medications at the index date had a lower risk of nonadherence than patients taking one class of antihypertensive medication (OR=0.79, CI=0.76–0.83).
Association between medication adherence and health outcomes
Table 3 shows the associations between antihypertensive medication adherence and adverse health outcomes using Cox’s proportional hazard model, which satisfied the proportionality assumption. After adjusting for gender, age, type of health insurance, CVD risk at baseline, diabetes, dyslipidemia, Charlson’s comorbidity score, any prior hospitalization and the number of classes of antihypertensive medications, the risk of all adverse health outcomes, which included both all-cause mortality and hospitalization for CVD, was 1.57-fold higher (HR: 1.57, CI: 1.40–1.76) in nonadherent patients than adherent patients.
We separately analyzed the associations between adherence to antihypertensive medication and all-cause mortality, hospitalization for CVD, hospitalization for stroke and hospitalization for IHD. After controlling for confounding variables, the risk in adherent patients was lower than the risk in nonadherent patients for both all-cause mortality (HR: 1.48, CI: 1.30–1.68) and hospitalization for CVD (HR: 1.25, CI: 1.12–1.39). In addition, as indicated in Table 3, the risk of hospitalization for stroke was 1.51-fold higher (HR: 1.51, CI: 1.29–1.77) in nonadherent patients. Moreover, the risk of hospitalization for IHD was 1.08-fold higher (HR: 1.08, CI: 0.90–1.29) in nonadherent patients, but this difference was not statistically significant.
Discussion
This study was designed to evaluate the association between medication adherence and all-cause mortality and hospitalization for CVD in people who were newly prescribed antihypertensive medications. We found that compared with adherence, nonadherence was significantly associated with an increase in adverse health outcomes. In this study, nonadherent patients had a 1.57-fold higher risk of all adverse health outcomes, including all-cause mortality and hospitalization for CVD. In separate analyses, the risks for all-cause mortality and hospitalization for CVD were also higher in nonadherent patients, by 1.48- and 1.25-fold, respectively, compared with adherent patients.
The results of this study are consistent with the results of prior studies, which showed that adherence decreased CVD-related outcomes.5, 6, 7, 8 Law et al.5 reported that blood pressure-lowering drugs were effective in preventing the risk of CVD in patients, regardless of whether they had CVD. Dragomir et al.6 showed similar results; when compared with high adherence (⩾80%), low adherence (<80%) increased the risk of coronary disease by 7% and the risk of chronic heart failure by 42%. Pittman et al.7 also reported that patients with a medication adherence of 80% or higher decreased their risk for CVD-related hospitalization by 33% (OR: 1.33, CI: 1.25–1.41) and emergency department visits by 45% (OR: 1.45, CI: 1.33–1.58). Further, according to a study from Taiwan, patients with low adherence (<80%) have a 43% higher risk of hospitalization for CVD than adherent patients (⩾80%).8 Similarly, low medication adherence has been associated with the risk of all-cause mortality,3, 18, 19 and nonadherence (<80%) to β-blockers or ACE inhibitors increases the risk of all-cause mortality by >1.5-fold.3 A meta-analysis has also reported that good adherence is associated with a reduced risk of mortality.18 Ho et al.3 assessed the relationship between CVD mortality and medication adherence in patients with coronary artery disease. They showed that medication nonadherence increased both the risk of CVD mortality and the risk of all-cause mortality. However, although both were increased by medication nonadherence, the risk of CVD mortality was not always higher than the risk of all-cause mortality. The increased risks of CVD mortality and all-cause mortality were dependent on the drug class taken by the patients. For example, nonadherence to β-blockers increased the risk of CVD mortality and the risk of all-cause mortality by 1.53- and 1.50-fold, respectively, and nonadherence to ACE inhibitors increased the risk of CVD mortality and the risk of all-cause mortality by 1.66- and 1.74-fold, respectively. In addition, the risk of all-cause mortality, which was increased by medication nonadherence (β-blockers: HR=1.50, ACE inhibitors: HR=1.74), was higher than the risk of CVD hospitalization, which was also increased by medication nonadherence (β-blockers: HR=1.10, ACE inhibitors: HR=1.40), regardless of the drug class. Other previous, related studies have shown similar results; low adherence increases the risk of all-cause mortality more than the risk of CVD-related hospitalization.3, 12, 17
We separately estimated the risk of stroke hospitalization and IHD hospitalization in nonadherent patients. The effect of low adherence to antihypertensive medication on stroke (HR=1.51) was greater than that on IHD. The association between adherence to antihypertensive medication and hospitalization for stroke has also been well documented in previous studies.6, 20, 21, 22 A meta-analysis has indicated that blood pressure-lowering drugs reduce the risk of CVD events by 24% and the risk of stroke events by 29% compared with placebo.21 Moreover, compared with adherence (⩾80%), nonadherence in newly diagnosed hypertensive patients has been reported to increase the risk of hospitalization for coronary disease by 13%, the risk of hospitalization for acute myocardial infarction by 15% and the risk of hospitalization for stroke by 28%.22
Prior studies on the association between medication adherence and health outcomes have reported similar results; however, the medication adherence rates and the proportion of adherence in the study populations have varied. In this study, 42.4% of the study population had high medication adherence (⩾80%) during the study period, and the mean medication adherence was 57.9%. The World Health Organization has reported that adherence to long-term antihypertensive drug treatment varies between 50 and 70%.15 In addition, Bramley et al.23 showed that hypertensive patients from 13 US health plans had a high mean MPR of 87%. The range of adherence proportions was 36–85%, with 35.6% in New Orleans, 61.7% among the beneficiaries of an HMO (Health Maintenance Organization) in the southwestern United States, 74% among the beneficiaries at a Veterans Affairs office and 85% in Taiwan.8, 24, 25 This difference in adherence to antihypertensive medication between studies stems from the populations studied, types of study design, drug classes, methods of adherence measurement, sources of data, definitions of adherence and components of adherence to medication.26, 27
The risk factors affecting nonadherence to antihypertensive medication in the present study were younger age, Medicaid health insurance, no diagnosis with diabetes or dyslipidemia, taking one class of antihypertensive medication and a history of hospitalization. Similarly, previous studies have found that increased age and comorbidities (that is, diabetes, dyslipidemia and obesity) are associated with adherence to antihypertensive medication.28, 29, 30 However, unlike these studies, there was no significant difference in adherence to antihypertensive medication between genders in our study. The difference in adherence to antihypertensive medication between genders observed in previous studies was likely because of the study populations, follow-up periods and other risk factors affecting medication adherence, such as education, race, social/family support and the healthcare system.28, 29, 31, 32, 33 Munger et al. have reported that the effects of gender on medication adherence are inconsistent across ethnic backgrounds.30 In South Korea, women showed higher nonadherence to antihypertensive medication than men (OR=0.97, CI=0.95–0.99) in a 1-year follow-up study. However, there was no difference in medication adherence between genders among hypertensive patients with disabilities.10, 34
We identified an association between medication adherence and hospitalization for CVD and mortality in hypertensive patients who were newly prescribed antihypertensive medication in South Korea. There are several limitations to this study. First, we indirectly measured adherence to antihypertensive medication based on administrative claims data. There are many different methods to measure adherence directly or indirectly. Direct methods allow researchers to directly observe patient therapy and/or measure the amount of medication taken, but they also have limitations because of patient’s tricks and variations in metabolism. In addition, it is difficult to apply direct methods to a large population.35 Indirect methods, such as using administrative data, are commonly used and more efficient when assessing medication adherence in a large population. The MPR method is one indirect method of calculating adherence using administrative data. The values of the MPR method were not determined based on whether patients actually took their medication according to the prescription but determined by the prescription written by physicians. Nevertheless, the MPR method is a well-validated measurement tool and is useful for measuring adherence over a long-term period; it is one of the best predictors of hospitalization using administrative data.11, 13, 36, 37
Second, although the administrative claims used in our study allow easy access to information for large populations, they do not include some other risk factors affecting CVD prognosis, such as smoking, family history of CVD, physical activity and socioeconomic status.38, 39 We used the number of different classes of antihypertensive medications prescribed on the index date instead of blood pressure values because our data did not contain any information on the clinical severity of hypertension, but a meta-analysis has indicated that lowering blood pressure using antihypertensive medication reduces coronary heart disease or stroke events, regardless of patient blood pressure.20, 5 Diagnoses of dyslipidemia and diabetes were considered proxy variables for blood cholesterol and glucose levels, and previous studies indicate that these variables affect the risk of CVD events.20
Third, the validity of the diagnoses may also be a limitation. To the best of the authors’ knowledge, studies on the validity of hypertension diagnosis using the KNHICD have not been conducted in South Korea. However, previous studies have suggested that the combination of a diagnosis of hypertension and prescriptions results in higher agreement between administrative claims and medical records/patient survey data than a diagnosis of hypertension alone or prescriptions alone.40, 41 Bullano et al.40 showed that the sensitivity, specificity and kappa score of hypertension defined using both diagnosis and prescription information were 76.2%, 93.3% and 0.65%, respectively, which were relatively high. In addition, Sokol et al.2 identified hypertensive patients as those who had at least two claims for outpatient services or one claim for hospitalization during 1 year and had at least one prescription, which was same as our definition of hypertensive patients. The condition of at least two claims for outpatient services was included to reduce the incidence of false-positive diagnoses. Therefore, our study used both diagnosis of disease and prescriptions for antihypertensive drugs to identify hypertensive patients. Nevertheless, we may have underestimated the number of hypertensive patients in the process of selecting the study population. For example, the KNHICD contains all hypertensive patients’ healthcare utilization data in South Korea, but these data do not include patients who did not visit clinics or hospitals because of low awareness of hypertension, limited physical conditions, lack of time or economic problems. In addition, hypertensive patients who had only one claim for outpatient services were not included.
Finally, although we assessed the association between medication adherence and all-cause mortality in our study, it may be more appropriate to assess CVD mortality as the outcome to evaluate the risk of low adherence to antihypertensive medication. However, medication adherence is directly and indirectly related to all-cause mortality.19 All-cause mortality, which intrinsically includes disease-specific mortality, is one important outcome that needs to be improved. Previous studies have reported similar results, demonstrating that low adherence is associated with an increased risk of all-cause mortality.3, 12, 17, 18
Even with these limitations, to our knowledge, this study is the first to measure the medication adherence rates of hypertensive patients over a 4-year period and to identify the effect of adherence to antihypertensive medication on hospitalization for CVD and all-cause mortality in South Korea.
In conclusion, low adherence to antihypertensive medication in hypertensive patients is associated with an increased risk of hospitalization for CVD and all-cause mortality. Although our results indicate that medication adherence is an important factor for the prevention of adverse health outcomes, the proportion of patients with adherence to long-term care was <50% in the studied population in South Korea. These findings suggest that intervention programs should be developed and designed to improve medication adherence in patients with low adherence. Further studies are needed to evaluate the effects of intervention programs on improving adherence.
References
Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, Wang J . Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res 2009; 32: 1032–1040.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS . Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 2005; 43: 521–530.
Ho PM, Magid DJ, Shetterly SM, Olson KL, Maddox TM, Peterson PN, Masoudi FA, Rumsfeld JS . Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J 2008; 155: 772–779.
Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM . The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract 2008; 62: 76–87.
Law MR, Morris JK, Wald NJ . Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009; 338: b1665.
Dragomir A, Cote R, Roy L, Blais L, Lalonde L, Berard A, Perreault S . Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Med Care 2010; 48: 418–425.
Pittman DG, Tao Z, Chen W, Stettin GD . Antihypertensive medication adherence and subsequent healthcare utilization and costs. Am J Manag Care 2010; 16: 568–576.
Wu PH, Yang CY, Yao ZL, Lin WZ, Wu LW, Chang CC . Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in Taiwan. Am J Hypertens 2010; 23: 155–160.
Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY . First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther 2009; 31: 1309–1320.
Park JH, Shin Y, Lee SY, Lee SI . Antihypertensive drug medication adherence and its affecting factors in South Korea. Int J Cardiol 2008; 128: 392–398.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC . Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin 2009; 25: 2303–2310.
Hong JS, Kang HC . Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea. Med Care 2011; 49: 378–384.
Halpern MT, Khan ZM, Schmier JK, Burnier M, Caro JJ, Cramer J, Daley WL, Gurwitz J, Hollenberg NK . Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension 2006; 47: 1039–1048.
Andrade SE, Kahler KH, Frech F, Chan KA . Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 2006; 15: 565–574.
WHO. Adherence to long-term therapies. World Health Organization: Geneva, Switzerland. 2003 pp 107–114.
Hansen RA, Kim MM, Song L, Tu W, Wu J, Murray MD . Comparison of methods to assess medication adherence and classify nonadherence. Ann Pharmacother 2009; 43: 413–422.
Degli Esposti L, Saragoni S, Batacchi P, Benemei S, Geppetti P, Sturani A, Buda S, Degli Esposti E . Adherence to statin treatment and health outcomes in an Italian cohort of newly treated patients: results from an administrative database analysis. Clin Ther 2012; 34: 190–199.
Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, Johnson JA . A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006; 333: 15.
Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, Krumholz HM, Rumsfeld JS . Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med 2006; 166: 1842–1847.
Kettani FZ, Dragomir A, Cote R, Roy L, Berard A, Blais L, Lalonde L, Moreau P, Perreault S . Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke 2009; 40: 213–220.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, Weiss NS . Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA 2003; 289: 2534–2544.
Breekveldt-Postma NS, Penning-van Beest FJ, Siiskonen SJ, Falvey H, Vincze G, Klungel OH, Herings RM . The effect of discontinuation of antihypertensives on the risk of acute myocardial infarction and stroke. Curr Med Res Opin 2008; 24: 121–127.
Bramley TJ, Gerbino PP, Nightengale BS, Frech-Tamas F . Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm 2006; 12: 239–245.
Piette JD, Heisler M, Ganoczy D, McCarthy JF, Valenstein M . Differential medication adherence among patients with schizophrenia and comorbid diabetes and hypertension. Psychiatr Serv 2007; 58: 207–212.
Paramore LC, Halpern MT, Lapuerta P, Hurley JS, Frost FJ, Fairchild DG, Bates D . Impact of poorly controlled hypertension on healthcare resource utilization and cost. Am J Manag Care 2001; 7: 389–398.
Krousel-Wood M, Thomas S, Muntner P, Morisky D . Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol 2004; 19: 357–362.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M . Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336: 1114–1117.
Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG . Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 2009; 120: 1598–1605.
Wong MC, Jiang JY, Griffiths SM . Factors associated with antihypertensive drug compliance in 83,884 Chinese patients: a cohort study. J Epidemiol Community Health 2010; 64: 895–901.
Munger MA, Van Tassell BW, LaFleur J . Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed 2007; 9: 58.
Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, Schwartz JS . Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 2005; 165: 1147–1152.
Grigoryan L, Pavlik VN, Hyman DJ . Predictors of antihypertensive medication adherence in two urban health-care systems. Am J Hypertens 2012; 25: 735–738.
Bailey JE, Hajjar M, Shoib B, Tang J, Ray MM, Wan JY . Risk factors associated with antihypertensive medication nonadherence in a statewide medicaid population. Am J Med Sci, (e-pub ahead of print 9 August 2013; doi:10.1097/MAJ.0b013e31825ce50f).
Park JH, Shin Y, Lee SY . Antihypertensive drug medication adherence of people with disabilities and its affecting factors in Korea. J Prev Med Public Health 2007; 40: 249–258.
Ho PM, Bryson CL, Rumsfeld JS . Medication adherence: its importance in cardiovascular outcomes. Circulation 2009; 119: 3028–3035.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC . An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med Care 2008; 46: 1125–1133.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC . Prospective validation of eight different adherence measures for use with administrative claims data among patients with schizophrenia. Value Health 2009; 12: 989–995.
Padwal R, Straus SE, McAlister FA . Evidence based management of hypertension. Cardiovascular risk factors and their effects on the decision to treat hypertension: evidence based review. BMJ 2001; 322: 977–980.
Hozawa A, Okamura T, Murakami Y, Kadowaki T, Nakamura K, Hayakawa T, Kita Y, Nakamura Y, Abbott RD, Okayama A, Ueshima H . Joint impact of smoking and hypertension on cardiovascular disease and all-cause mortality in Japan: NIPPON DATA80, a 19-year follow-up. Hypertens Res 2007; 30: 1169–1175.
Bullano MF, Kamat S, Willey VJ, Barlas S, Watson DJ, Brenneman SK . Agreement between administrative claims and the medical record in identifying patients with a diagnosis of hypertension. Med Care 2006; 44: 486–490.
Quam L, Ellis LB, Venus P, Clouse J, Taylor CG, Leatherman S . Using claims data for epidemiologic research. The concordance of claims-based criteria with the medical record and patient survey for identifying a hypertensive population. Med Care 1993; 31: 498–507.
Acknowledgements
This paper was supported by the Health Insurance Review and Assessment Service (HIRA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, S., Song, H., Oh, SK. et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res 36, 1000–1005 (2013). https://doi.org/10.1038/hr.2013.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.85
Keywords
This article is cited by
-
Antihypertensive medication nonadherence and target organ damage in children with chronic kidney disease
Pediatric Nephrology (2024)
-
Evaluating the effect of the COVID-19 pandemic on hypertension and diabetes care in South Korea: an interrupted time series analysis
BMC Public Health (2023)
-
Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems
Nature Reviews Drug Discovery (2023)
-
Association of Remote Patient Monitoring with Mortality and Healthcare Utilization in Hypertensive Patients: a Medicare Claims–Based Study
Journal of General Internal Medicine (2023)
-
Association between health literacy and medication adherence in chronic diseases: a recent systematic review
International Journal of Clinical Pharmacy (2023)