Abstract
Purpose
Demands on publicly funded ophthalmic services worldwide continue to increase with new treatments, waiting time targets, working time limits, and restricted budgets. These highlight the necessity to develop innovative ways of utilising existing capacity more effectively.
Method
A new regional, fully electronic ophthalmic-referral service with digital imaging was trialled using existing information-technology (IT) infrastructure. Following successful pilot study, the service was rolled out regionally. Service delivery data was prospectively collated for all the attendances in the year prior to (2006) and the year following (2008) introduction.
Results
Comparing 2006 against 2008, median waiting times reduced (14 vs 4 weeks), and fewer new patients were observed (8714 vs 7462 P<0.0001), with 1359 referrals receiving electronic diagnosis (e-diagnosis). New patient did not arrive (635 vs 503 P<0.0001) and emergencies also reduced (2671 v 1984 P<0.0001).
Discussion
Novel use of existing IT infrastructure improves communication between primary and secondary care. This promotes more effective use of limited outpatient capacity by retaining patients with non-progressive, asymptomatic pathology in the community, whilst fast-tracking patients with sight-threatening disease. Resultant significant, sustained improvements in regional service delivery point to a simple model that could easily be adopted by other providers of universal healthcare globally.
Similar content being viewed by others
Introduction
Globally and publicly funded health-care systems are challenged by long waits from the referral.1 Predictably, evidence shows that shorter waits have population-wide benefits,2 including in ophthalmology.3 The UK Department of Health recently introduced short waiting-time guidelines for outpatient appointments.4 Similar targets have been set by universal health-care providers worldwide.5 These changes have implications for hospital eye services (HES), whose outpatients constitute 10% of all the general hospital outpatients.6 Pressure on outpatient services have escalated due to increasing patient numbers, educational restructuring, working-time directives, and fiscal constraints.7 Together, these highlight the need to use existing resources more effectively.
This study describes changes to a regional ophthalmic service with six consultants serving a population of 400 000 in Fife, Scotland. The region includes three ophthalmic-hospital sites, 50 optometry practices, and 250 general practitioners (GPs). We follow the establishment of a centralised ophthalmic electronic referral unit (COERU), which uses digital images for clinical decision making.
In 2005, the maximum outpatient wait from the referral was 38 weeks, placing Fife in fifth position across the fourteen Scottish health boards. An internal audit of 400 new glaucoma patients showed that patients risked sight loss due to delayed appointments.8 The audit also highlighted significant inefficiencies in the referral pathway contributing to delay.
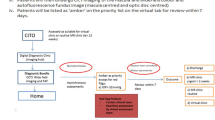
At this time, >90% of patients followed the traditional referral pathway involving community optometry examination of patients with a report posted to the GP. The GP then married the patient’s medical history to the optometry report and posted the complete referral to one of the three hospitals. The referrals arrived at the general medical-records departments to be sent on to the ophthalmology department. Referrals were then arbitrarily divided into six piles, awaiting consultant vetting during their weekly visits to each hospital. Further delays ensued due to consultant leave, absence of GP or optometry information, and inter-consultant referral. (Figure 1) The audit also identified that many patients were returned to the community after a single outpatient visit with advice and no active treatment. These practices pointed to the need for improved communication between primary and secondary care to enable improved patient journeys.
Illustrates differences between the original paper-based referral pathway in 2006, which had a lengthy paper trail, referral delay, and considerable cross referral as patients were arbitrarily allocated to consultants by untrained medical records staff. The new pathway shows the improved electronic referral system with reduction in the number of steps required for final outcome, and illustrates the two way nature of communication between primary and secondary care.
Materials and methods
Pilot study
Following the audit findings, a suggestion was made to enhance the speed and accuracy of communication between primary and secondary care, thereby reducing the paper trail by using electronic referral with digital images. This was piloted by extending existing encrypted NHS email access to three optometric practices (July 2005–January 2007). Consecutive electronic referrals (346) were studied with attached JPEG formatted digital images when relevant. GPs forwarded patients’ medical histories simultaneously using an existing secure Scottish wide (IT link, SciGateway (Scottish clinical information gateway)).
The pilot study showed that electronic referral was feasible, fast, and obviated the need for outpatient appointment in 128 (37%) patients. The 128 cases included dry age-related macular degeneration (ARMD) (35, 27%), non visually threatening retinal lesions (30,23%), corneal and conjunctival abnormalities (14, 11%), and glaucoma suspects (12, 9%). Thirty-one (8.9%) of the original cohort of 346 patients were deemed to require an urgent appointment, and these were patients with wet ARMD, advanced glaucoma, papilloedema, and retinal vascular pathology. To establish clinical safety, all patients were examined in hospital within 6 weeks by two ophthalmologists. Clinical agreement with electronic diagnosis was achieved in 124 cases (97%). There were, however, four cases of disagreement between clinical and e-diagnosis that highlighted the inadequacies of depth and field in digital images. Referral protocols have since been adjusted accordingly. Importantly, there was a high patient satisfaction (97%) with the new system.9
Centralised ophthalmic electronic referral unit (COERU)
The compelling pilot data catalysed roll out of the pilot to the entire region. In May 2007, electronic referral was rolled out regionally, following several training sessions for GPs and optometrists. A new electronic referral form was designed incorporating more clearly defined clinical and diagnostic criteria, with particular attention paid to cataract, ARMD, and glaucoma. Previous HES attendance details were also incorporated, as the pilot had shown that 16% of patients had attended the HES within 3 years of current referral. Referrals were accepted at a single site with specialist nurse vetting and appointments within 48 h.
The British Medical Association confirmed that NHS mail had approved for transfer of confidential patient information, and the General Medical Council and Medical Protection Society confirmed that additional security or indemnity arrangements were unnecessary.
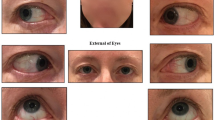
Figure 2 shows fundus examples of patients that were electronically referred and diagnosed.
Examples of patients that were electronically referred and diagnosed. The first was a case of pediatric papilloedema that was transferred from an outlying region to a central pediatric unit within 2 h of community examination and electronic referral (upper two fundus photographs). The second was a case of longstanding myopic degeneration in an asymptomatic patient that did not require hospital examination and was discharged to community followup (lower two fundus photographs).
Results
Following the introduction of COERU, waiting times reduced from a median of 14–4 weeks (Table 1). The introduction of electronic referral did not significantly increase referral rate (8707 vs 8821). Significantly fewer new patients were observed in 2008 (7462 vs 8714). There were fewer casualities (1984 vs 2671) and ‘did not arrive’ (DNA) patients (503 vs 635) in 2008. Collectively, the department saw 1359 less new, 687 less unscheduled and saved, 132 new DNA appointments saving 2178 new appointments in 2008. New appointments in Scotland during this period cost £110,10 and hence this represented a simple estimated saving of £239 580 per annum for new appointments. Additionally, Fife has a geographically widespread population, and other savings may have accrued from reduced transport expenses for patients and the NHS. An example is that the average cost of hospital transport was £30 per visit in Fife. Approximately 20% of patients required hospital transport. The amount calculated to be saved is £13 068 (435 × £30) in transport for new appointments. Other financial benefits would also accrue from reduced unnecessary appointments including reduction of lost economic productivity of patients who are employed although these were not looked into in this study. Financial benefit from reduced new appointments may have been offset by 2489 more followup appointments during this period (cost £90),10 mainly from the newly set up macular degeneration treatment clinics costing a total of £224 010.
In order to address clinical safety issues that may arise from the new referral pathway, a monthly clinical governance meeting was set up to discuss adverse events, near misses, and misdiagnoses. Information was dispersed to GPs and optometrists in COERU support meetings. To assist the clinical governance meetings, a database was set up with clinical audit trail for 18 months of all patients given e-diagnosis and not physically seen in hospital. Of the 1359 patients not seen following electronic referral between May 2008 and April 2009, 12 patients attended before April 2011. Reasons included specific patient request (four cases), duplicate GP referral (five cases), and clerical error (three cases). The departmental complaint rate has reduced from 7.5 to 3.5 per annum with none related to COERU. There have been no reported adverse events. COERU continues to run with over 5 years experience and 50 000 referrals with all trends above sustained. Through auditing, we found that medical and nursing time allocation’s workload has altered following commencement of COERU (Table 2). Very few referrals were rejected as a consequence of poor quality of image, and when this occurred the most common reason was treatable cataract, which required referral, as systems set in place were similar to those for the diabetic retinopathy screening programme.
Discussion
Previous work has independently shown the benefits of electronic referral in reducing outpatient workload,11 reducing waiting times,12 and matching of diagnostic accuracy.13 We believe our service is the first to completely incorporate electronic referral with digital images into a regional ophthalmic service with long-term service delivery results.
Improving two-way communication through novel use of currently available secure IT technology between hospital and community practice, dramatically reduced steps in the referral pathway with shorter waiting times. Improved clinical information enabled more appropriate use of hospital resources. As noted in other reports, shortened outpatient waits indirectly resulted in fewer DNAs14, 15 and emergencies, as we found in our study.16 We believe this to be an indirect result of short waiting times, more appropriate allocation of patient’s first hospital visit to specialist clinic and identification of asymptomatic, non-sight threatening pathology that is retained in the community.
Key lessons included careful piloting and auditing of every step with active stakeholder involvement from the beginning. Shortcutting these steps have resulted in failure of other ophthalmology electronic referral systems.17 A significant difference between Scotland and the rest of the United Kingdoms is the higher community remuneration for sight tests. We and other groups have shown the service benefits from this.18
Encrypted mail is freely available across the NHS in the United Kingdoms. Similar encrypted email technology can easily and cheaply be adapted for the purpose of using secured hypertext transport protocols (HTTPs) to encrypt information as has already been used internationally for telemedicine.19, 20 Pockets of electronic referral already exist within ophthalmology globally.21, 22 Furthermore, electronic referral has been shown to have lower startup costs than conventional services.23 This may hold even greater benefit for developing countries and regions with geographically dispersed populations.
Across Fife, we have found benefits to be profound. Fife now has the shortest outpatient waits of any ophthalmology region in Scotland, and has the shortest wait for hospital appointments for wet macular-degeneration patients amongst 40 European centres.24 Our findings are highly relevant as the impact of improved electronic communication between primary and secondary ophthalmic care is likely to increase further in the near future, following the Scottish government passing a £6.6 million business case to connect all community optometrists to hospital ophthalmology departments in 2010. The platform will use a ‘virtual private network’ (VPN) that connects to a server and will provide secure, remote access to community optometrists. Twelve of the fourteen Scottish healthboards have already agreed to connect to the network at present. The results of these changes will be available in the near future, and may have implications for other UK regions as well as international providers of ophthalmic healthcare.
In summary, we show that ophthalmic service redesign based around a core of structured, centralised electronic referral with increased clinical information, has the potential to improve the use of existing capacity with resultant beneficial effects on waiting times, reductions in DNA rate, and emergency attendances.

References
Siciliani L, Hurst J . Tackling excessive waiting times for elective surgery: a comparative analysis of policies in 12 OECD countries. Health Policy 2005; 72 (2): 201–215.
Cooper ZN, Mcguire A, Jones S, Le Grand J . Equity, waiting times, and NHS reforms: retrospective study. BMJ 2009; 339: b3264.
Guyer DR, Fine SL, Maguire MG, Hawkins BS, Owens SL, Murphy RP . Subfoveal choroidal neovascular membranes in age-related macular degeneration. Visual prognosis in eyes with relatively good initial visual acuity. Arch Ophthalmol 1986; 104 (5): 702–705.
The NHS Improvement Plan: Putting people at the heart of public services., Department of Health,(UK) Editor 2004..
Willcox S, Seddon M, Dunn S, Edwards RT, Pearse J, Tu JV . Measuring and reducing waiting times: a cross-national comparison of strategies. Health Aff (Millwood) 2007; 26 (4): 1078–1087.
The Royal College Ophthalmologists. Ophthalmic Services Guidance: ophthalmic outpatients departments. February 2012; Available from http://www.rcophth.ac.uk/page.asp?section=293sectionTitle=Ophthalmic+Services+Guidance.
Buyx AM, Friedrich DR, Schone-Seifert B . Ethics and effectiveness: rationing healthcare by thresholds of minimum effectiveness. BMJ 2011; 342: d54.
Imrie F, Blaikie A, Cobb C, Sinclair A, Wilson D, Dobson S et al. Glaucoma electronic patient record--design, experience and study of high-risk patients. Eye (Lond) 2005; 19 (9): 956–962.
Cameron JR, Ahmed S, Curry P, Forrest G, Sanders R . Impact of direct electronic optometric referral with ocular imaging to a hospital eye service. Eye (Lond) 2009; 23 (5): 1134–1140.
The Official Project Initiation Document for 18 Weeks: the Referral to Treatment Standard Includes And An Overview Of The Programme, Timeline, And Key Deliverables. 2008 February 2012; The British Government. Available from http://www.18weeks.scot.nhs.uk/key-18-weeks-documents/.
Baldwin L, Clarke M, Hands L, Knott M, Jones R . The effect of telemedicine on consultation time. J Telemed Telecare 2003; 9 (Suppl 1): S71–S73.
Whited JD, Hall RP, Foy ME, Marbrey LE, Grambow SC, Dudley TK et al. Teledermatology's impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health 2002; 8 (3): 313–321.
Chao LW, Cestari TF, Bakos L, Oliveira MR, Miot HA, Zampese M et al. Evaluation of an Internet-based teledermatology system. J Telemed Telecare 2003; 9 (Suppl 1): S9–12.
Gallucci G, Swartz W, Hackerman F . Impact of the wait for an initial appointment on the rate of kept appointments at a mental health center. Psychiatr Serv 2005; 56 (3): 344–346.
Cohen AD, Kaplan DM, Kraus M, Rubinshtein E, Vardy DA . Nonattendance of adult otolaryngology patients for scheduled appointments. J Laryngol Otol 2007; 121 (3): 258–261.
Hau S, Ioannidis A, Masaoutis P, Verma S . Patterns of ophthalmological complaints presenting to a dedicated ophthalmic accident & emergency department: inappropriate use and patients' perspective. Emerg Med J 2008; 25 (11): 740–744.
de Bont A, Bal R . Telemedicine in interdisciplinary work practices: on an IT system that met the criteria for success set out by its sponsors, yet failed to become part of every-day clinical routines. BMC Med Inform Decis Mak 2008; 8: 47.
Ang GS, Ng WS, Azuara-Blanco A . The influence of the new general ophthalmic services (GOS) contract in optometrist referrals for glaucoma in Scotland. Eye (Lond) 2009; 23 (2): 351–355.
Hersh D, Hersch F, Mikuletic L, Neilson S . A Web-based approach to low-cost telemedicine. J Telemed Telecare 2003; 9 (Suppl 2): S24–S26.
Liederman EM, Morefield CS . Web messaging: a new tool for patient-physician communication. J Am Med Inform Assoc 2003; 10 (3): 260–270.
Kumar S, Yogesan K, Hudson B, Tay-Kearney ML, Constable IJ . Emergency eye care in rural Australia: role of internet. Eye (Lond) 2006; 20 (12): 1342–1344.
John S, Sengupta S, Reddy SJ, Prabhu P, Kirubanandan K, Badrinath SS . The Sankara Nethralaya mobile teleophthalmology model for comprehensive eye care delivery in rural India. Telemed J E Health 2012; 18 (5): 382–387.
Bergmo TS . An economic analysis of teleconsultation in otorhinolaryngology. J Telemed Telecare 1997; 3 (4): 194–199.
Scottish Advisory Board Meeting (ARMD). 2010.
Acknowledgements
Thanks to Fife optometrists Colin Ferrier, Kirit Rach, Charles McKinnon, Ruth Robertson, Helen Paterson, Graham West (Fife Specialist ophthalmic nurses), Dr James Cameron, and Dr Suheb Ahmed for work on the pilot study. No funding was obtained for the research described. The pilot study was funded by the Electronic Clinical and Communications Implementation project (Scottish government).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Borooah, S., Grant, B., Blaikie, A. et al. Using electronic referral with digital imaging between primary and secondary ophthalmic services: a long term prospective analysis of regional service redesign. Eye 27, 392–397 (2013). https://doi.org/10.1038/eye.2012.278
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.278
Keywords
This article is cited by
-
A Proposed Framework for Machine Learning-Aided Triage in Public Specialty Ophthalmology Clinics in Hong Kong
Ophthalmology and Therapy (2021)
-
Contribution of a synchronic teleneurology program to decrease the patient number waiting for a first consultation and their waiting time in Chile
BMC Medical Informatics and Decision Making (2020)
-
A categorisation of problems and solutions to improve patient referrals from primary to specialty care
BMC Health Services Research (2018)
-
A comparative study of glaucoma referrals in Southeast Scotland: effect of the new general ophthalmic service contract, Eyecare integration pilot programme and NICE guidelines
BMC Ophthalmology (2015)