ABSTRACT
BACKGROUND
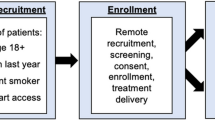
Tobacco treatment is underused in primary care. We designed a Tobacco Care Management system to increase the delivery of treatment and reduce the burden on primary care providers (PCPs). A one-click functionality added to the electronic health record (EHR) allowed PCPs to refer smokers to a centralized tobacco treatment coordinator (TTC) who called smokers, provided brief counseling, connected them to ongoing treatment and gave feedback to PCPs.
OBJECTIVE
To study the system’s feasibility and acceptability among PCPs, and its utilization by smokers.
DESIGN
Using a mixed methods design, we documented system utilization quantitatively from February 1, 2010 to July 31, 2011, and conducted two focus groups with PCPs in June 2011.
PARTICIPANTS
Thirty-six PCPs and 2,894 smokers from two community health centers in Massachusetts.
MAIN MEASURES
Quantitative: One-click referral utilization by PCPs, proportion of smokers referred and connected to treatment. Qualitative: PCPs’ reasons for use, barriers to use, and experiences with feedback.
KEY RESULTS
Twenty-nine PCPs (81 %) used the functionality more than once, generating 466 referrals for 15 % of known smokers seen during the study. The TTC reached 260 (56 %) of the referrals and connected 135 (29 %) to additional treatment. The director of one center sent PCPs monthly feedback about their utilization compared to peers. These PCPs referred a greater proportion of their known smokers (18 % vs. 9 %, p < 0.0001) and reported that monthly feedback motivated referrals. PCPs attending focus groups (n = 24) appreciated the system’s simplicity, access to updated resources, and time-efficient way to address smoking, and wanted more feedback about cessation outcomes. They collectively supported the system’s continuation.
CONCLUSIONS
A novel EHR-based Tobacco Care Management system was adopted by PCPs, especially those receiving performance feedback, and connected one-third of referred smokers to treatment. The model has the potential to improve the delivery and outcomes of evidence-based tobacco treatment in primary care.


Similar content being viewed by others
REFERENCES
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–45.
Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–8.
Centers for Disease Control and Prevention. Quitting smoking among adults—United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1513–9.
Fiore MC, Jaen CR, Baker T, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update. In: Clinical Practice Guideline. Rockville: U.S. Department of Health and Human Services. Public Health Service; 2008.
Quinn VP, Stevens VJ, Hollis JF, Rigotti NA, Solberg LI, Gordon N, et al. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am J Prev Med. 2005;29(2):77–84.
Benowitz NL. Chronic disease management approach to treating tobacco addiction: comment on “nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit”. Arch Intern Med. 2011;171(21):1907–9.
Schroeder SA. What to do with a patient who smokes. JAMA. 2005;294(4):482–7.
American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. March 2007. www.medicalhomeinfo.org/Joint%20Statement.pdf. Accessed June 29, 2012.
Sherman SE, Takahashi N, Kalra P, Gifford E, Finney JW, Canfield J, et al. Care coordination to increase referrals to smoking cessation telephone counseling: a demonstration project. Am J Manag Care. 2008;14(3):141–8.
Bentz CJ, Bayley KB, Bonin KE, Fleming L, Hollis JF, Hunt JS, et al. Provider feedback to improve 5A’s tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res. 2007;9(3):341–9.
An LC, Bluhm JH, Foldes SS, Alesci NL, Klatt CM, Center BA, et al. A randomized trial of a pay-for-performance program targeting clinician referral to a state tobacco quitline. Arch Intern Med. 2008;168(18):1993–9.
Rothemich SF, Woolf SH, Johnson RE, Devers KJ, Flores SK, Villars P, et al. Promoting primary care smoking-cessation support with quitlines: the QuitLink Randomized Controlled Trial. Am J Prev Med. 2010;38(4):367–74.
Borland R, Balmford J, Bishop N, Segan C, Piterman L, McKay-Brown L, et al. In-practice management versus quitline referral for enhancing smoking cessation in general practice: a cluster randomized trial. Fam Pract. 2008;25(5):382–9.
Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Haas JS. An electronic health record-based intervention to improve tobacco treatment in primary care: a cluster-randomized controlled trial. Arch Intern Med. 2009;169(8):781–7.
Willett JG, Hood NE, Burns EK, Swetlick JL, Wilson SM, Lang DA, et al. Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics. Am J Prev Med. 2009;36(4):337–40.
Sheffer MA, Baker TB, Fraser DL, Adsit RT, McAfee TA, Fiore MC. Fax referrals, academic detailing, and tobacco quitline use a randomized trial. Am J Prev Med. 2012;42(1):21–8.
Cantrell J, Shelley D. Implementing a fax referral program for quitline smoking cessation services in urban health centers: a qualitative study. BMC Fam Pract. 2009;10:81.
Bernstein SL, Jearld S, Prasad D, Bax P, Bauer U. Rapid implementation of a smokers’ quitline fax referral service in an urban area. J Health Care Poor Underserved. 2009;20(1):55–63.
Centers for Disease Control and Prevention. Vital signs: current cigarette smoking among adults aged ≥18 years—United States, 2005–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1207–12.
Barry M, Saul J, Bailey L. U.S. quitlines at a crossroads: Utilization, budget, and service trends 2005–2010. Phoenix, Arizona: 2010 Contract No.: SR-01.
Carpenter MJ, Hughes JR, Gray KM, Wahlquist AE, Saladin ME, Alberg AJ. Nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit: a randomized clinical trial. Arch Intern Med. 2011;171(21):1901–7.
Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–4.
Zhu SH, Anderson CM, Tedeschi GJ, Rosbrook B, Johnson CE, Byrd M, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347(14):1087–93.
Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850.
Acknowledgements
We are grateful for the participation of the Community Health Centers, and wish to thank Southern Jamaica Plain Health Center, Charlestown Health Center, Michael Lambert, MD, and Mark Eisenberg, MD. We would also like to acknowledge Elizabeth Mort, MD, MPH and Partners HealthCare System’s High Performance Medicine for support of the project.
Partners Healthcare, Inc. funded the Tobacco Care Management program and supported the Tobacco Care coordinator. Dr. Kruse’s effort was supported by grant #T32HP12706-03-00 from the Health Resources and Services Administration for the Harvard General Medicine Fellowship. Dr. Rigotti’s effort was supported by NIH grant #K24-HL08880. The funders of these grants had no role in study design, conduct, data analysis, interpretation, or manuscript preparation, review, or approval.
An earlier version of this information was accepted for presentation as a poster at the Society for Research in Nicotine and Tobacco 18th Annual Meeting, Houston, Texas, March 15, 2012 and the Society for General Internal Medicine 35th Annual Meeting, Orlando, Florida May 12, 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest. Nancy A. Rigotti reports unpaid consultancy for Pfizer and Alere Wellbeing, research grants to MGH from Nabi Biopharmaceuticals and Pfizer, and royalties from UpToDate.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kruse, G.R., Kelley, J.H.K., Linder, J.A. et al. Implementation of an Electronic Health Record-Based Care Management System to Improve Tobacco Treatment. J GEN INTERN MED 27, 1690–1696 (2012). https://doi.org/10.1007/s11606-012-2174-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2174-6