Abstract
Purpose
To determine the effect of electronic prescribing (EP) with a clinical information system (Intellivue Clinical Information Portfolio, Philips, UK) on prescribing errors and omitted doses in a paediatric intensive care unit (PICU).
Methods
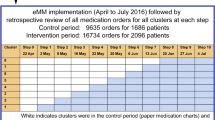
Prospective audit of prescribing errors and omitted doses for 96 h periods in three epochs: (1) before implementation of EP, (2) 1 week and (3) 6 months later.
Results
There was a non-significant reduction in prescribing errors: 8.8% (95% CI 4.4–13.2) pre-implementation of EP versus 8.1% (4.4–11.8) 1 week after implementation and 4.6% (2.0–7.2) 6 months later. The prevalence of omitted doses decreased significantly 6 months following implementation, changing from 8.1% (5.8–10.4) pre-implementation to 10.6% (6.5–14.7) 1 week after implementation and 1.4% (CI 0–2.8%) 6 months after implementation (P < 0.05).
Conclusion
EP within a clinical information system increases medication safety in a PICU.
Similar content being viewed by others
References
Sammons H, Conroy S (2008) How do we ensure safe prescribing for children? Arch Dis Child 93:98–99
Ghaleb MA, Barber M, Franklin BD, Wong ICK (2010) The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child 95:113–118
van Rosse F, Maat B, Rademaker CM, van Vught AJ, Egberts AC, Bollen CW (2009) The effect of computerized physician order entry on medication prescription errors and clinical outcome in pediatric and intensive care: a systematic review. Pediatrics 123:1184–1190
Shulman R, Singer M, Goldstone J, Bellingan G (2005) Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care 9:516–521
Thiru K, Rowe S, Shaw N, Durward A, Inwald DP, Ramnayaran P (2010) Survey of clinical information system usage by paediatric intensive care units in the UK. Intensive Care Med 36:1616–1617
Walsh KE, Adams WG, Bauchner H, Vinci RJ, Chessare JB, Cooper MR, Herbert PM, Schainker EG, Landrigan CP (2006) Medication errors related to computerized order entry for children. Pediatrics 118:1872–1879
Acknowledgments
Dr Inwald is grateful for support from the NIHR Biomedical Research Centre funding scheme. The Centre for Medication Safety and Service Quality is affiliated to the Centre for Patient Safety and Service Quality at Imperial College Healthcare NHS Trust which is funded by the National Institute of Health Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Warrick, C., Naik, H., Avis, S. et al. A clinical information system reduces medication errors in paediatric intensive care. Intensive Care Med 37, 691–694 (2011). https://doi.org/10.1007/s00134-010-2126-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2126-8